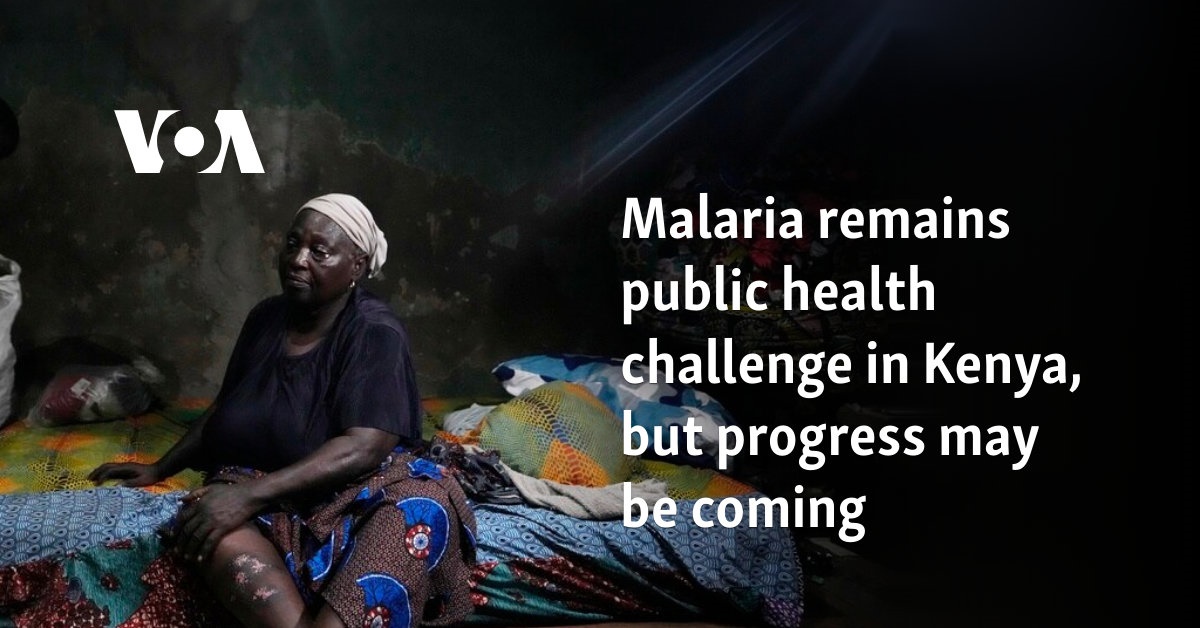
As the coffin bearing the body of Rosebella Awuor was lowered into the grave, heart-wrenching sobs from mourners filled the air. Her sister Winnie Akinyi, the guardian to Awuor’s orphaned son, fell to the ground, wailing.
It was the latest of five deaths in this family attributed to malaria. The disease is common in Kenya, and it is preventable and curable, but poverty makes it deadly for those who can’t afford treatment.
In the family’s compound in the western county of Migori, three other graves are visible, that of Awuor’s husband and their other two children who died from malaria before age 2.
Awuor, 31, fell ill in December and lost her five-month pregnancy before succumbing to malaria. Her 11-year-old son is the family’s only survivor.
Malaria is still a significant public health challenge in Kenya, though some progress may be coming. Parts of Kenya participated in an important pilot of the world’s first malaria vaccine, with a reported drop in deaths for children under 5. Kenya’s health ministry hasn’t said when the vaccine will be widely available.
The biggest impact is felt in regions characterized by high temperatures like Kenya’s Indian Ocean coast, and places with high rainfall like the western region near Lake Victoria.
Kenya had an estimated 5 million malaria cases and more than 12,000 deaths reported in 2022, according to the World Health Organization. The WHO has declared April 25 as World Malaria Day.
Most of those affected are children under 5 and pregnant women.
New approaches needed
Kenya continues to combat malaria with traditional methods such as distributing bed nets that are treated with insecticides, spraying breeding areas, and promoting early diagnosis and treatment, but experts say progress against the disease with those approaches has plateaued.
Public health expert Dr. Willis Akhwale, special adviser for the Kenya End Malaria Council, said the COVID-19 pandemic slowed the distribution of drugs and treatment.
He said innovative treatment methods are needed in the wake of drug-resistant cases reported in parts of Africa.
“We need to start looking at investments in new-generation medicines. That should then be able to counter any resistance in [the] foreseeable future,” he said.
Akhwale said other needs include more funding and logistical support.
“In Kenya, the shortfall in terms of the need is almost $52 million, so we need to close that gap,” he said, citing health ministry data. He recommended domestic funding and private sector support amid donor fatigue with crises around the world.
Wilson Otieno has been admitted to a hospital three times for malaria and has received outpatient treatment countless times. It’s expensive for the 33-year-old accountant and father in the lakeside city of Kisumu.
Malaria is never “pocket friendly,” he said.
Some progress has been made with local manufacturing of crucial medication.
The Kenya-based Universal Corporation Limited last year received the WHO’s approval to produce an antimalarial drug known as Spaq, a combination of sulfadoxine-pyrimethamine plus amodiaquine.
The approval was an important step in Africa’s capacity to make lifesaving medications, a new focus for governments and public health officials after vulnerabilities were exposed by the COVID-19 pandemic. Africa relies heavily on drug imports.
“It will really help in lowering the dependency for imports as we saw during the COVID era, where whatever was being imported actually had huge supply disruptions,” said Palu Dhanani, the founder and managing director of UCL.
If you don’t get the right medicine at the right time, malaria can cause unnecessary deaths, Dhanani said.