Each year, around 50,000 patients worldwide require a bone marrow transplant to treat various blood cancers and disorders, with 2,000 of these cases originating from the UK. These transplants are often a critical, life-saving procedure for individuals suffering from conditions like leukemia, lymphoma, and other serious blood diseases. However, finding a matching donor remains a significant challenge due to the need for genetic compatibility. We spoke with Dr Rahul Bhargava, Director and Chief BMT, Fortis Memorial Research Institute (Gurugram) to understand the the various aspects and importance of raising awareness and encouraging more people to register as bone marrow donors globally.
Why is World Marrow Donor Day significant, and how does it help raise awareness about the need for more donors?
World Marrow Donor Day raises global awareness about the importance of registering as a donor, as finding a matching donor can be a challenge due to the need for genetic compatibility. By celebrating donors, survivors, and the efforts of registries worldwide, the event encourages more people to join donor registries, helping to increase the chances for patients to find life-saving matches. It also serves to educate the public on the donation process, dispelling myths and emphasising the relatively simple steps involved, which can ultimately save lives.
Can you explain how the matching process works for marrow transplants, and what factors are considered when selecting a donor?
The matching process for marrow transplants is based on finding a close match in the human leukocyte antigen (HLA) proteins, which are markers on the surface of cells that help the immune system recognise its cells versus foreign ones. For a successful transplant, the patient’s and donor’s HLA types need to closely match to prevent the immune system from rejecting the donor cells. Doctors typically look for at least 8 to 10 key HLA markers to align. A sibling may have the highest chance of being a match, but if no family match is found, registries of unrelated donors are searched. Since HLA types are inherited, ethnic background plays a role, and a diverse registry increases the chances of finding a match. Other factors like the donor’s age, overall health, and even blood type are also considered to ensure the best outcome. A close match reduces the risk of complications like graft-versus-host disease, where the donor cells attack the patient’s body, making this a critical step in the transplant process.
What is the significance of Human Leukocyte Antigen (HLA) compatibility in marrow transplants, and how often are perfect matches found?
Human Leukocyte Antigen (HLA) compatibility is crucial in marrow transplants because HLA markers help the immune system distinguish between its cells and foreign invaders. For a successful transplant, the donor’s and patient’s HLA markers must closely match. If the HLA types are not compatible, the patient’s immune system might reject the transplanted cells or the donor’s cells might attack the patient’s body, leading to serious complications like graft-versus-host disease (GVHD). A close HLA match significantly improves the chances of the body accepting the transplant, reducing the risk of rejection and complications.
However, finding a perfect HLA match can be challenging. Among siblings, there is about a 25% chance of being a perfect match, but only around 30% of patients have a matching sibling. For those without a family match, finding a perfect match from an unrelated donor is even more difficult. The likelihood of finding a perfect match in the general population depends on ethnic background, with some groups having better representation in donor registries than others. In many cases, close matches are used instead of perfect ones, but the closer the match, the better the transplant outcome.
What are the recent advancements in marrow transplantation techniques that have improved patient outcomes?
Following are recent advancements in marrow transplantation techniques in India that have improved patient outcomes:
Haploidentical Transplants: Use of stem cells from partially matched family members has expanded donor options and increased the chances of successful transplants.
Cord Blood Transplants: Growth of cord blood banks allows for the use of umbilical cord stem cells, providing more matches for patients without a perfect donor.
Enhanced Stem Cell Processing: Advances in processing and cryopreservation techniques have improved the quality and viability of stem cells used in transplants.
Novel Conditioning Regimens: The development of reduced-intensity conditioning treatments has minimized treatment-related toxicity and improved patient safety.
Improved GVHD Management: New therapies and strategies for managing graft-versus-host disease have reduced complications and enhanced patient quality of life.
Personalised Medicine: The adoption of genomic profiling helps tailor treatments to individual patient needs, increasing transplant success rates.
Increased Training and Collaboration: Enhanced training for healthcare professionals and partnerships with international institutions have led to better practices and outcomes.
How has technology and research evolved to reduce complications like graft-versus-host disease (GVHD) in marrow transplants?
Technology and research have evolved to reduce graft-versus-host disease (GVHD) in marrow transplants through several key advancements:
Improved Donor Matching: Enhanced genetic testing provides more accurate HLA matching between donor and recipient, reducing the risk of GVHD.
Advanced Conditioning Regimens: Newer conditioning regimens use lower doses of chemotherapy and radiation, which are less toxic to the patient and reduce the risk of severe GVHD while still effectively preparing the patient for the transplant.
Better Immunosuppressive Drugs: Modern medications specifically target the immune cells responsible for GVHD, improving management while minimizing side effects.
T-cell Depletion: Techniques like T-cell depletion remove or reduce the number of T-cells from the donor’s marrow or stem cells before transplant. These T-cells are primarily responsible for causing GVHD, so reducing their number helps lower the risk.
Enhanced Prevention Protocols: Updated GVHD prevention strategies use a combination of drugs and therapies tailored to individual needs.
Early Detection and Monitoring: Advanced monitoring methods allow for the early detection of GVHD, leading to prompt treatment and less severe complications. These advancements collectively improve the ability to manage GVHD, leading to better outcomes for patients undergoing marrow transplants.
How does diversity in donor registries affect the success of finding matches for patients from different ethnic backgrounds?
Diversity in donor registries plays a critical role in increasing the chances of finding successful matches for patients from different ethnic backgrounds. The reason lies in the human leukocyte antigen (HLA) system, which is used to match patients with donors. HLA markers are inherited, so they are more likely to be similar among people of the same ethnic background. Since every person’s HLA type is unique, patients from minority or mixed ethnic groups have a harder time finding matches if their specific HLA types are underrepresented in the registry. Hence, making it significant to raise awareness and encourage more and more people to sign up with bone marrow registries.
What role do you think emerging therapies, such as gene editing or regenerative medicine, will play in the future of marrow transplantation?
Gene Editing is a technology that allows scientists to make precise changes to the DNA of an organism. One popular tool for this is CRISPR-Cas9, which acts like molecular scissors, cutting the DNA at a specific spot and allowing scientists to either repair or replace a genetic sequence. In medicine, this technology can be used to fix mutations that cause genetic diseases, essentially allowing doctors to “edit out” harmful genes. This has huge potential for treating inherited disorders like sickle cell anemia or certain cancers by repairing a patient’s own cells.
Regenerative Medicine, on the other hand, focuses on repairing or replacing damaged tissues and organs using advanced techniques like stem cell therapy or tissue engineering. The idea is to harness the body’s natural healing abilities by stimulating the regeneration of tissues or by growing new tissues in a lab that can be transplanted into patients. For example, if a person’s bone marrow is damaged, regenerative medicine could eventually allow scientists to grow new, healthy marrow from the patient’s own cells.
In the context of marrow transplantation, gene editing and regenerative medicine offer exciting possibilities for the future:
Gene Editing: Instead of relying on donor stem cells, gene editing could correct defective genes in a patient’s own stem cells. For example, a person with a genetic blood disorder could have their stem cells edited to remove the harmful mutation. These repaired cells could then be transplanted back into the patient, effectively curing the disease without needing a donor match or risking rejection.
Regenerative Medicine: This could enable scientists to grow healthy bone marrow or blood stem cells in a lab. In the future, patients might not need to wait for a donor match—scientists could generate new bone marrow from a patient’s own cells, which would be a perfect match, eliminating the risk of immune rejection. It could also make transplants more widely available, as lab-grown stem cells could provide a consistent supply for patients in need.
Together, these fields could make marrow transplantation more personalized, reduce the need for donor matches, and improve treatment outcomes for many blood-related diseases.
How can innovations like cord blood transplants and haploidentical transplants benefit patients who lack a fully matched donor?
Cord Blood Transplants involve using stem cells collected from the umbilical cord and placenta after a baby is born. These stem cells can be used to replace damaged bone marrow in patients. Because cord blood stem cells are less mature, they are more forgiving of mismatches in HLA typing, making them a good option for patients who don’t have a perfectly matched donor.
While Haploidentical Transplants use stem cells from a family member who is only partially matched (sharing 50% of the same HLA markers). This approach allows patients to use stem cells from relatives, such as parents or siblings, even if they aren’t a perfect match. Advanced techniques help reduce risks like graft-versus-host disease and improve outcomes.
Both innovations help patients find suitable donors more quickly. Cord blood transplants provide a readily available source of stem cells with less stringent matching requirements, while haploidentical transplants expand the donor pool by allowing the use of partially matched family members. This increases the chances of successful transplants for patients who otherwise might not find a fully matched donor.
What is the process of becoming a marrow donor, and what should potential donors know about the procedure and recovery?
Becoming a marrow donor involves several steps to ensure that you are a suitable match for a patient in need. Here’s a step-by-step breakdown of the process:
Register: Sign up online with a marrow donor registry
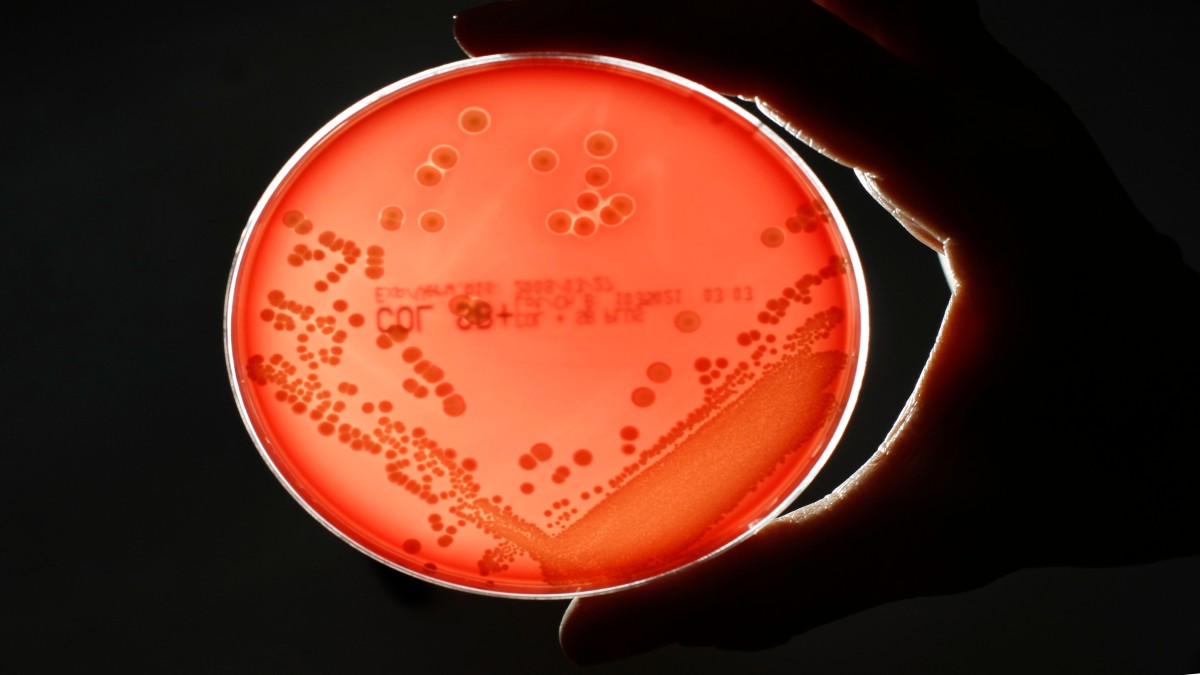
Swab Sample: Provide a cheek swab or blood sample for HLA typing to determine your tissue type.
Wait for a Match: Your HLA type will be added to the registry, and you’ll wait until you’re matched with a patient in need.
Confirm Match: If matched, provide a blood sample and undergo a health check to confirm compatibility.
Consent: Once confirmed the donation process will be explained in detail, including potential risks and the type of donation required. The donor will need to give formal consent to proceed with the donation.
Donate: Depending on the patient’s needs, you’ll either donate through a Peripheral Blood Stem Cell (PBSC) procedure or a Bone Marrow Donation (a surgical method).
Recover: After donation, you’ll typically recover within a few days to two weeks, depending on the method used.
Potential bone marrow donors should know that the donation process is generally safe and involves two main methods: Peripheral Blood Stem Cell (PBSC) donation or bone marrow extraction. PBSC donation is non-surgical and involves receiving medication for several days to boost stem cell production, followed by a procedure similar to donating blood. Bone marrow extraction, however, is a surgical procedure done under anesthesia, where marrow is taken from the pelvic bone using a needle. Donors may feel soreness in the lower back or fatigue afterward, but most recover fully within a week or two. Both procedures are well-monitored, and donors receive follow-up care to ensure they are healing well.

)





)